Phlebitis (fli-BY-tis) is a serious venous inflammation caused when the blood vessel walls are damaged. This damage can be caused by injury, trauma or infection to your veins.
Thrombophlebitis (throm-bow-fli-BY-tis) is caused by one or several blood clots in a vein, causing inflammation. The condition can cause pain and irritation, as it prevents proper circulation.
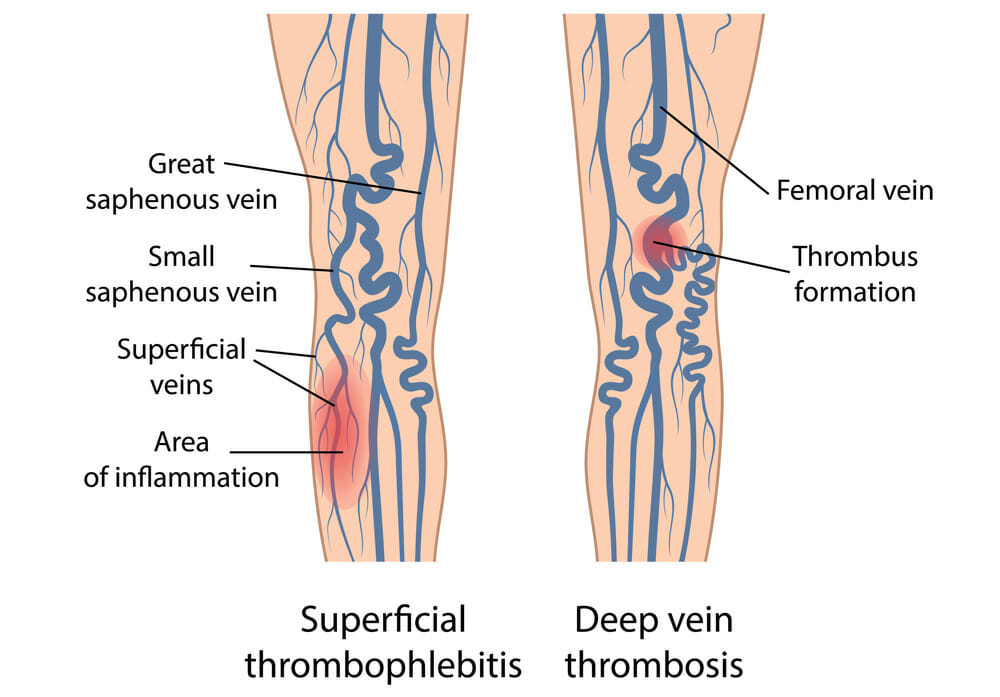
Varicose veins and phlebitis may appear similar, but the latter can cause serious complications that risk your health. Fortunately, it can be treated if detected early. Phlebitis can be superficial, meaning it affects the veins in the surface of your skin, or it can develop in your deep veins, which is known as deep vein thrombophlebitis, or deep vein thrombosis (DVT).
Superficial phlebitis is rarely serious, and will often resolve quickly, unlike deep vein thrombosis. If you have DVT, large blood clots can form and potentially travel to your lungs, resulting in a life-threatening condition known as pulmonary embolism.
What causes Superficial Phlebitis?
Superficial phlebitis is often caused by a complication of a medical or surgical procedure, which has injured the vein. Deep vein thrombophlebitis can be caused by a number of hereditary, medical or lifestyle factors. For example, if you are pregnant, have just given birth, use birth control or hormone replacement therapy, your chances of phlebitis are increased.
Other factors, such as age and previous medical history, can contribute to its development. Prolonged periods of inactivity will increase your risk, whether it is because of long-haul travel, or an inactive lifestyle.
If you have large varicose veins your risk of developing phlebitis is higher in particular after long-distance flights.
What is phlebitis and how is it diagnosed?
Phlebitis can be detected from a blood test or an ultrasound, that assess blood flow and blockage. The blood test, known as a D-dimer, measures a substance that is released when a blood clot deteriorates. If during the test this substance is not detected, it is unlikely a blood clot has developed. During an ultrasound, clots and blockages can be seen, as the probe is pressed against your skin. The scan will also assess if the clot has extended to the deep system of veins.
A venogram can also be used to identify blood clots, in smaller veins. However, it is more invasive than a D-dimer or ultrasound, as it involves injecting a specific dye into your veins, that appears during an x-ray.
How long does Phlebitis last?
If you have phlebitis, your leg or arm will likely become tender, with redness appearing over the affected area. It may also feel hot to the touch and increasingly itchy, and begin to throb or burn.
Symptoms include burning, itching and swelling which tend to be worse in the lower legs as they are furthest from your heart and harder for the blood to circulate.
Severe cases of phlebitis can result in chest pain and fever. If phlebitis goes undetected, skin discolouration and ulcers can occur.
Varicose veins can also develop due to phlebitis. The symptoms are similar, with swelling, itching and aching to be expected. Although not life-threatening, varicose veins can cause your veins to twist and protrude against the skin and can be generally uncomfortable.
If you are experiencing swelling, tenderness, itching or a burning sensation, be sure to contact a medical professional to assess your risk of phlebitis, or other underlying health issues.
Read more: Is it possible for vein damage to heal?
Phlebitis Treatment
- Walking is recommended, as it helps increasing the blood flow and therefore prevents blood clots from developing
- Anti-inflammatory drug for phlebitis treatment: if you are diagnosed with superficial phlebitis, you might be recommended to take aspirin or ibuprofen, which will alleviate the pain and inflammation
- Compression stockings (knee or thigh high) improve your blood flow and may help to relieve your pain and swelling
- Professional phlebitis treatment: in case of a Deep Vein Thrombosis (DVT), you may have to receive a treatment in order to make sure that no complications occur. This may include antibiotics and/or anticoagulant.
In any case, always consult a professional before taking any medication.
Seek expert advice
The doctors at The Vein Institute specialise in varicose vein treatment. We offer patients a comprehensive program using non-surgical laser treatment techniques. You can learn more in our Definitive Guide to Varicose Vein Treatment.
The benefits of non-surgical varicose vein treatment are:
- Walk-in walk-out treatment
- 98% success rate
- Extremely effective
- Can be performed at a clinic (no hospitalisation)
- No general anaesthetic
- Medicare rebates apply
- No downtime or time away from work
Call us on 04 2010 2637, or fill out our booking request form.