In Australia, almost two million people have diabetes, with an estimated 5.1 per cent of the population affected. While diabetes affects different parts of the body in different ways, the core nature of diabetes affects the blood and blood vessels, which links it very closely to venous disorders like varicose veins.
Diabetes is a condition which affects the body’s ability to regulate healthy amounts of glucose (sugar) in your blood. When unmanaged, the blood in a diabetic’s body can become thicker, making it harder for the blood to flow properly through the body. The effects can exacerbate any existing issues and trigger dormant underlying conditions affecting the veins, leading to an increased deterioration in health.
Is there a link between diabetes and varicose veins?
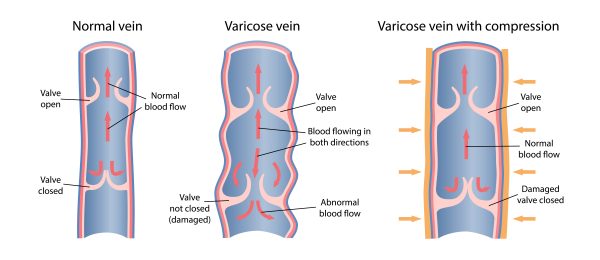
Varicose veins have a variety of causes, including genetics, excess weight, poor diet and lifestyle. When these occur, veins in the legs become weak and struggle to pump blood back up to the heart (CVI). Although it is not a direct cause of varicose veins, there is a link between the associated effects of diabetes adding additional pressure to the veins and possibly amplifying preexisting venous disorders.
Diabetes, excess weight and obesity are all closely related, with most people suffering from type 1 diabetes prone to weight gain. While those suffering from type 2 diabetes are often already overweight. Excess weight puts a strain on the veins in your legs, weakens the blood vessels and often leads to the development of varicose veins.
Diabetes is also associated with increased blood sugar levels, causing the blood to become thicker. This can cause already strained veins to struggle to push blood up the legs, heal sores and fight infections. As a result, those with diabetes are at increased risk of developing varicose veins, and those who already have both are at increased risk of developing even more serious health problems like ulcers, soft tissue damage and chronic vein problems.
What can I do as a diabetic?
While this can be overwhelming to take in, especially when you’re already trying to manage diabetes itself, taking care of your veins as a diabetic can be easier than it sounds. Some key tips for those with type 1 or 2 diabetes to help manage their veins include
- Focusing on a low salt, low alcohol diet.
- Maintaining regular medication and management of diabetes itself, as directed by your doctor.
- Exercise regularly to keep the muscles around the veins healthy and manage weight levels.
- Wear compression stockings in cases where you’re seated for extended periods of time (working at a desk, travelling in the car or plane)
If you already have varicose veins and are concerned about how to treat them, fear not! There’s a range of treatment options for the management and removal of varicose veins.
- A combination of strict diet, application of creams and targeted stretching and exercise in mild cases.
- Endovenous Laser Ablation, which uses a laser fibre inserted into the unhealthy veins to seal them off and channel the blood into stronger veins.
- Radiofrequency Ablation, which is a similar procedure to Endovenous Laser however it uses radiofrequency to seal the damaged veins.
Seek expert advice
The doctors at The Vein Institute specialise in varicose vein treatment. We offer patients a comprehensive program using non-surgical laser treatment techniques. You can learn more in our Definitive Guide to Varicose Vein Treatment.
The benefits of non-surgical varicose vein treatment are:
- Walk-in walk-out treatment
- 98% success rate
- Extremely effective
- Can be performed at a clinic (no hospitalisation)
- No general anaesthetic
- Medicare rebates apply
- No downtime or time away from work
Call us on 04 2010 2637, or fill out our booking request form.


